Contents
- Introduction to Depression
- Causes and Risk Factors
- Signs and Symptoms
- Types of Depression
- Diagnosis and Assessment
- Treatment and Management
- Living with Depression
- Support Systems
- Depression in Special Populations
- Resources and Further Reading
Introduction to Depression
Depression, also known as major depressive disorder (MDD), is a common and serious mental health condition characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in activities. It affects a person’s thoughts, feelings, and behaviors, leading to emotional and physical symptoms that can significantly impact daily life.
Prevalence and Impact
Depression is a widespread global issue, affecting millions of people of all ages, genders, and backgrounds. According to the World Health Organization (WHO), depression affects 5% of individuals worldwide. This means that roughly 280M people suffer from the condition and it is more common among women than men. It not only affects an individual’s quality of life but also has a substantial economic impact due to lost productivity and healthcare costs.
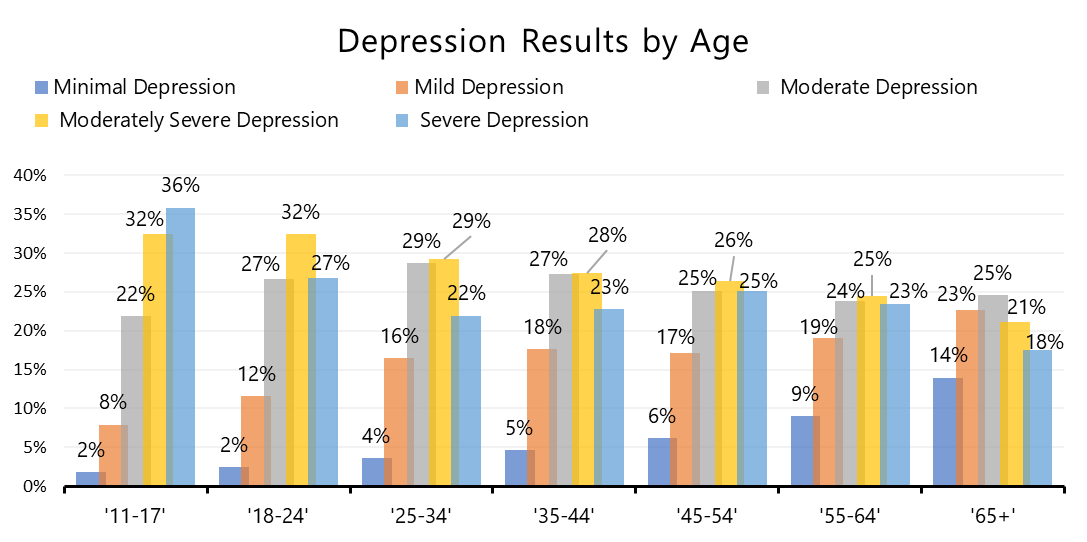
https://www.mhanational.org/online-depression-screening-data-and-statistics
The Importance of Seeking Help
One of the challenges in addressing depression is that individuals often suffer in silence, fearing stigma or misunderstanding. However, seeking help is crucial, as depression is a treatable condition. With the right support and treatment, individuals with depression can lead fulfilling lives.
Causes and Risk Factors
Biological Factors
Depression is believed to involve changes in brain chemistry and structure. Neurotransmitters, such as serotonin and norepinephrine, play a role in regulating mood, and imbalances in these chemicals can contribute to depression.
Psychological Factors
Psychological factors, including negative thought patterns, low self-esteem, and unresolved trauma, can increase the risk of developing depression. Stressful life events, such as loss, trauma, or relationship difficulties, can also trigger depressive episodes.
Environmental Factors
Environmental factors, such as a lack of social support, financial difficulties, or exposure to chronic stressors, can contribute to depression. Living in a disadvantaged socioeconomic environment can increase vulnerability.
Genetics and Family History
There is evidence to suggest that depression may have a genetic component. Individuals with a family history of depression may be at a higher risk of developing the condition themselves.
Signs and Symptoms
Depression can manifest in a variety of ways, and symptoms may vary from person to person. It is important to recognize these signs to seek help when needed.
Emotional Symptoms
- Persistent sadness
- Feelings of hopelessness or despair
- Irritability
- Guilt or worthlessness
- Loss of interest or pleasure in activities
Cognitive Symptoms
- Difficulty concentrating or making decisions.
- Memory problems
- Negative thinking patterns, including suicidal thoughts.
Physical Symptoms
- Changes in appetite and weight
- Sleep disturbances (insomnia or excessive sleep)
- Fatigue or lack of energy
- Physical aches and pains with no clear cause
Behavioral Symptoms
- Withdrawal from social activities
- Reduced productivity at work or school
- Avoidance of responsibilities
- Self-destructive behaviors
Types of Depression
- Major Depressive Disorder (MDD), often referred to simply as “depression,” is a common and serious mental health condition characterized by persistent and profound feelings of sadness, hopelessness, and a loss of interest or pleasure in most activities. It is more than just occasional feelings of sadness; it represents a prolonged and severe disruption of a person’s emotional and cognitive functioning.
- Persistent Depressive Disorder, also known as Dysthymia, is a type of chronic and long-lasting depressive disorder that differs from Major Depressive Disorder (MDD) primarily in terms of duration and severity. While MDD is characterized by severe depressive episodes that may last for weeks or months, Persistent Depressive Disorder involves a more prolonged and milder form of depression.
- Seasonal Affective Disorder (SAD) is a type of depression that occurs at the same time of year annually. The most common is the winter depression that starts in the fall and goes through to early spring. SAD has only been recognized since 1985 and tends to occur more frequently the further away from the equator people live. People diagnosed with SAD is around 5%, but upwards of 20% of people can have some symptoms of SAD. It occurs four times more often in women than men and the average age of onset seems to be around 23 years old. Symptoms can start out mild at the beginning of the season and worsen as the season goes on.
- Postpartum depression (PPD), also known as postnatal depression, is a type of depressive disorder that can affect individuals after giving birth, typically within the first year after childbirth. PPD is characterized by a range of emotional and physical symptoms that can be severe and long-lasting, significantly impacting a new parent’s ability to care for themselves and their baby. It is important to note that postpartum depression can also affect individuals who have experienced a miscarriage or stillbirth.
Diagnosis and Assessment
Diagnostic Criteria
Diagnosing depression typically involves a mental health professional assessing a person’s symptoms, duration, and severity. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) provides criteria for diagnosing depression.
Screening Tools
Several screening tools, such as the Patient Health Questionnaire-9 (PHQ-9) and the Beck Depression Inventory (BDI), are used to assess the presence and severity of depression.
Medical Evaluation
A thorough medical evaluation is important to rule out any underlying medical conditions that could mimic depressive symptoms, such as thyroid disorders or vitamin deficiencies.
Differential Diagnosis
Depression can co-occur with other mental health disorders, such as anxiety, which may require different treatment approaches. Accurate diagnosis is essential for effective treatment planning.
Treatment and Management
Psychotherapy
Psychotherapy, or talk therapy, is a cornerstone of depression treatment. Cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and dialectical-behavior therapy (DBT) are effective approaches for addressing depression.
Medications
Antidepressant medications, including selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), can help rebalance brain chemistry and alleviate depressive symptoms.
Lifestyle Changes
Adopting a healthy lifestyle can support recovery from depression. Regular exercise, a balanced diet, adequate sleep, and stress management techniques can all be beneficial.
Support Groups
A depression support group is a structured and safe space where individuals who are dealing with depression can come together to share their experiences, offer mutual support, and learn coping strategies for managing their condition. These groups are typically led by mental health professionals or trained facilitators and can be an essential part of a comprehensive treatment plan for depression. Here are some key aspects of depression support groups:
Alternative and Complementary Approaches
Some individuals find relief from depression symptoms through practices like yoga, meditation, acupuncture, and herbal supplements. These approaches should be used in conjunction with evidence-based treatments.
Prevention
- Risk Reduction – Reducing risk factors for depression, such as managing stress, maintaining a healthy lifestyle, and seeking treatment for underlying medical conditions, can help prevent the onset of the disorder.
- Early Intervention – Recognizing and addressing depressive symptoms early can prevent the condition from worsening. Encouraging open communication about mental health within families and communities is crucial.
- Building Resilience – Building emotional resilience through skills like problem-solving, coping strategies, and social support can help individuals better manage life’s challenges and reduce vulnerability to depression.
Living with Depression
Coping Strategies
Coping with depression can be challenging, but there are various strategies and techniques that can help individuals manage their symptoms and improve their overall well-being. It’s important to remember that coping strategies may vary from person to person, and what works for one individual may not work for another. Here are some effective coping strategies for depression:
- Self-Care – Prioritize self-care activities, including getting enough sleep, maintaining a healthy diet, and engaging in regular physical exercise. Physical activity has been shown to have a positive impact on mood.
- Mindfulness and Meditation – Practice mindfulness and meditation to help manage negative thought patterns and reduce stress. These techniques can improve self-awareness and emotional regulation.
- Set Realistic Goals – Break tasks into smaller, manageable steps. Setting achievable goals, even if they are small, can provide a sense of accomplishment and motivation.
- Routine – Establish a daily routine that includes regular sleep patterns and consistent mealtimes. A structured routine can provide a sense of stability and control.
- Limit Stress – Identify and manage sources of stress in your life. Techniques such as deep breathing exercises, progressive muscle relaxation, and stress-reduction strategies can be helpful.
- Avoid Alcohol and Substance Abuse – Alcohol and drugs can worsen depression symptoms. Limit or avoid their use and seek help if you have substance abuse issues.
- Positive Social Connections – Maintain connections with supportive friends and family members. Isolation can exacerbate depression, so reach out and spend time with loved ones.
- Limit Exposure to Negative Influences – Reduce exposure to negative news, social media, or individuals who may contribute to feelings of sadness or anxiety.
- Hobbies and Interests – Engage in activities you enjoy and that give you a sense of purpose. Pursuing hobbies and interests can improve mood and increase feelings of fulfillment.
Support Systems
Depression support systems are crucial for individuals dealing with depression. These systems provide emotional, practical, and social support to help those with depression cope with their condition and work towards recovery. Here are key components of a depression support system:
- Family and Friends – Loved ones can provide valuable emotional support and a listening ear. They can also help with daily tasks and encourage treatment compliance.
- Therapists and Counselors – Mental health professionals, such as therapists and counselors, offer structured support through psychotherapy. They provide strategies for managing depression and can help individuals gain insight into their thoughts and behaviors.
- Support Groups – Joining a depression support group allows individuals to connect with others who understand their experiences. It provides a sense of belonging and the opportunity to share coping strategies.
- Online Communities – Online forums and communities can be a source of support, especially for those who may have difficulty accessing in-person resources. Websites and social media groups focused on mental health provide a platform for sharing experiences and finding advice.
- Community and Faith-Based Organizations – Local organizations and religious groups may offer support, counseling, and community outreach programs that can be beneficial for those seeking help.
Depression in Special Populations
Children and Adolescents
Depression can affect individuals of all ages, including children and adolescents. Depression in young people is a serious mental health concern that requires attention and support. While the symptoms of depression in children and adolescents may be like those in adults, they can also manifest in unique ways. Here’s what you need to know about depression in children and adolescents:
Older Adults
Depression in older adults, often referred to as late-life depression or geriatric depression, is a common but frequently underdiagnosed and undertreated mental health condition. Older adults can experience depression for various reasons, and it presents unique challenges due to factors such as physical health problems, isolation, and life changes.
LGBTQ+ Community
Depression in the LGBTQ+ community is a significant concern, as individuals who identify as lesbian, gay, bisexual, transgender, queer, or other non-heteronormative sexual orientations or gender identities may face unique stressors and mental health challenges. Discrimination, stigma, and the experience of being a marginalized group can contribute to increased rates of depression among LGBTQ+ individuals. Here are key considerations regarding depression in the LGBTQ+ community:
Cultural Considerations
Cultural considerations play a significant role in how depression is perceived, experienced, and addressed. Cultural factors can influence how individuals, families, and communities understand and respond to mental health conditions like depression. It’s essential for mental health professionals to be culturally competent and sensitive to these factors when providing care.
Resources and Further Reading
Hotlines and Helplines
- National Suicide Prevention Lifeline: 1-800-273-8255
- Crisis Text Line: Text “HOME” to 741741
- National Alliance on Mental Illness (NAMI) Helpline: 1-800-950-NAMI (6264)
Books
- “The Noonday Demon: An Atlas of Depression” by Andrew Solomon
- “Feeling Good: The New Mood Therapy” by David D. Burns
- “The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a Time” by Alex Korb
Websites
- National Institute of Mental Health (NIMH):
- Depression and Bipolar Support Alliance (DBSA)
- Mental Health America (MHA)
- World Health Organization – Thinking Healthy
Support Organizations
- National Alliance on Mental Illness (NAMI)
- Anxiety and Depression Association of America (ADAA)
- American Foundation for Suicide Prevention (AFSP)

This comprehensive guide serves as a valuable resource for understanding depression, its causes, symptoms, treatment options, and ways to support individuals affected by this challenging condition. Depression is a treatable condition, and with the right knowledge and support, individuals can find hope and healing on their journey to recovery.