Table of Contents
INTRODUCTION
Psychiatry is the branch of medicine that focuses on the assessment, diagnosis, treatment, and prevention of mental health issues and disorders. Approximately 20% of the US population is dealing with mental health issues at any given time. That means nearly 1 in 5 people are struggling, suffering, and being negatively affected by their mental health issues. These issues affect them emotionally, mentally, occupationally, and relationally. Psychiatrists and psychiatric nurse practitioners are professionals whose main objective is to meet with individuals and families and help provide relief from issues. The field of psychiatry is operated by medical doctors (MD or DO) and psychiatric mental health nurse practitioners (PMHNP) who have advanced and specialized skills and training in treating mental health issues. They are trained in the medical model and approach the assessment of mental health issues from a biological, genetic, and chemical perspective. They typically utilize pharmacological medications to address these issues.
Purpose of the Guide
This guide is designed to provide a clear and concise overview of psychiatry for students, healthcare professionals, and anyone interested in understanding the mental health field. It aims to demystify psychiatric practices, introduce common psychiatric disorders, and discuss modern treatment approaches. Additionally, the guide seeks to encourage informed discussions about mental health, advocating for empathy and effective care in the treatment of mental health conditions.
Overview of Content Sections
The content of this guide is organized into several key sections. The first section delves into the history of psychiatry and how it has evolved over the years. Following this, there is a detailed discussion of various psychiatric disorders, categorized by their symptoms and impacts on daily life. The next section covers diagnostic methods and treatment strategies, including both pharmacological and psychotherapeutic options. Finally, the guide concludes with a look at the challenges and future directions in psychiatry, highlighting ongoing research and emerging trends in the field. This structure is designed to provide readers with a comprehensive understanding of psychiatry, from basic concepts to advanced applications.
UNDERSTANDING PSYCHIATRY
The history of psychiatry is a testament to the evolving understanding of mental health. From the ancient belief in supernatural influences to the development of modern science-based practices, psychiatry has undergone significant transformations. In the 18th and 19th centuries, the establishment of asylums marked the beginning of institutionalized care, although often with a focus on confinement rather than treatment. The 20th century brought the advent of psychoanalysis, pioneered by figures like Sigmund Freud, and later, the introduction of psychotropic medications revolutionized treatment options. Today, the field continues to evolve with advances in neuroscience and genetics, shaping a more nuanced understanding of mental health disorders.
Contemporary Scope and Role
In contemporary settings, psychiatry plays a pivotal role in healthcare by addressing a wide range of mental illnesses, from depression and anxiety to schizophrenia and bipolar disorder. Psychiatrists use a variety of tools to diagnose and treat patients, including medical examinations, psychological testing, and counseling sessions. The scope of psychiatry also extends to prevention and education, aiming to reduce the incidence of mental health issues and increase awareness about them. In addition, psychiatrists often collaborate with other healthcare professionals to provide holistic care, recognizing the interplay between psychological and physical health.
Integration with Other Medical Disciplines
Integrating psychiatry with other medical disciplines is crucial for delivering comprehensive healthcare. This interdisciplinary approach includes collaboration with neurology, considering the overlap in brain function and disorders; internal medicine, addressing physical conditions that can affect mental health; and pediatrics, focusing on the developmental aspects of child and adolescent psychiatry. Additionally, psychiatry intersects with social work, psychology, and nursing to ensure a broad spectrum of patient support and care. This integration facilitates a deeper understanding of the multifaceted nature of mental health and enhances the effectiveness of treatment plans tailored to individual needs.
TYPES OF MENTAL HEALTH DISORDERS
Anxiety disorders form a category of mental health diagnoses that lead to excessive nervousness, fear, apprehension, and worry. These disorders alter how a person processes emotions and behaves, also causing physical symptoms. Mild anxiety might be vague and unsettling, while severe anxiety may seriously affect day-to-day living. Here’s a detailed look at the various types of anxiety disorders:
- Generalized Anxiety Disorder (GAD) – Generalized Anxiety Disorder is characterized by chronic anxiety, excessive worry, and tension, even when there is little or nothing to provoke it. Individuals with GAD may anticipate disaster and be overly concerned about health, money, family problems, or difficulties at work. Even though they usually realize that their anxiety is more intense than the situation warrants, they can’t let go of their concerns.
- Panic Disorder – This disorder involves sudden and repeated episodes of intense fear that peak within minutes. These episodes are known as panic attacks and are accompanied by physical symptoms that may include chest pain, heart palpitations, shortness of breath, dizziness, or abdominal distress. A specific event can trigger these attacks or may occur unexpectedly, and they often lead individuals to worry about future attacks and avoid places where they might appear.
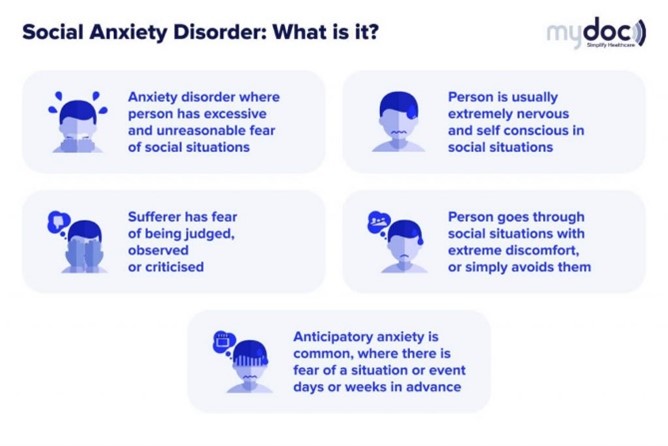
- Social Anxiety Disorder – Social anxiety disorder involves overwhelming worry and self-consciousness about everyday social situations. The worry often centers on a fear of being judged by others or behaving in a way that might cause embarrassment or lead to ridicule. This can extend to various situations—from speaking at a public event to engaging in casual conversations.
- Agoraphobia – It involves a fear of being in places where escape might be difficult or that help wouldn’t be available if things go wrong. Many people misunderstand this condition as a simple fear of open spaces, but it is more complex, often involving a fear of crowds, bridges, or of being outside alone.
- Separation Anxiety Disorder – Though most commonly seen in children, adults can also develop separation anxiety disorder, which is the fear of being away from home or loved ones. Individuals with this disorder often worry excessively about being apart from family members or others to whom they are attached.
Mood Disorders
Mood disorders, also known as affective disorders, are a category of mental health conditions characterized by severe disturbances in a person’s mood and emotional state. These disturbances can significantly impact an individual’s quality of life, affecting their ability to function and maintain relationships. Here’s a detailed exploration of the various types of mood disorders:
- Major Depressive Disorder (MDD) – Major Depressive Disorder is characterized by a pervasive and persistent low mood accompanied by low self-esteem and a loss of interest or pleasure in normally enjoyable activities. Symptoms must last at least two weeks for a diagnosis of MDD and can include significant weight loss or gain, insomnia or hypersomnia, fatigue, feelings of worthlessness, impaired concentration, and recurrent thoughts of death or suicide.
- Bipolar Disorder – This is marked by dramatic shifts in a person’s mood, energy, and ability to think clearly. These mood swings can range from highs (mania or hypomania) to lows (depression). During a manic phase, an individual may feel excessively euphoric, irritable, or energized, often resulting in impulsive decisions and poor judgment. During a depressive phase, the individual may experience symptoms similar to those of major depression. Bipolar disorder is often categorized into several types, including Bipolar I, Bipolar II, and Cyclothymic Disorder, depending on the nature and severity of mood swings.

Source: Baton Rough Behavioral Health
- Dysthymia (Persistent Depressive Disorder) – Dysthymia is a chronic form of depression that lasts for at least two years (one year in children and adolescents). Although its symptoms are not as severe as major depression, the long duration and persistent nature of dysthymia can significantly impair functioning and well-being. Individuals with dysthymia may experience symptoms such as poor appetite or overeating, insomnia or hypersomnia, low energy, low self-esteem, poor concentration, and feelings of hopelessness.
- Seasonal Affective Disorder (SAD) – This is a type of depression that occurs at the same time of year annually. The most common is the winter depression, which starts in the fall and continues to early spring. SAD has only been recognized since 1985 and tends to occur more frequently the further away people live from the equator. People diagnosed with SAD are around 5%, but upwards of 20% of people can have some symptoms of SAD. It occurs four times more often in women than men, and the average age of onset seems to be around 23 years old. Symptoms can start mild at the beginning of the season and worsen as the season goes on.
Psychotic Disorders
Psychotic disorders represent a group of serious mental health conditions that affect the mind, distorting a person’s thinking, perceptions, emotions, and behaviors. These disorders are characterized by symptoms known as psychosis, including delusions (false beliefs that are not based in reality) and hallucinations (seeing or hearing things that are not there). Other symptoms can include disorganized thinking, a lack of motivation, and reduced social engagement. Here’s a detailed look at the primary types of psychotic disorders:
- Schizophrenia – It is a chronic, severe, and disabling brain disorder that affects about 1% of the population worldwide. It is characterized by two key features: hallucinations and delusions. Hallucinations can be of any type, but visual and auditory are the most common. Delusions are beliefs outside the scope of probable situations, such as believing the government is conspiring against you or that you are some famous person. Although there are treatments for schizophrenia, most people will have to cope with some symptoms throughout their lives. It affects men and women equally; onset is generally in late teens or early 20’s but could occur as late as 30-45 years old.
- Schizoaffective Disorder – This disorder is a condition that includes symptoms of both schizophrenia and a mood disorder (either major depression or bipolar disorder). The psychotic symptoms are persistent even without mood disorder symptoms, and the mood symptoms are prominent.
- Brief Psychotic Disorder – This disorder involves sudden, short periods of psychotic behavior, often in response to a highly stressful event, such as a death in the family. Symptoms, which include hallucinations, delusions, or disorganized speech or behavior, last less than a month, with individuals returning to full baseline functioning after the episode.
- Delusional Disorder – Delusional disorder is characterized by the presence of delusions, which are unshakeable beliefs in something untrue or not based on reality. These delusions typically involve real-life situations that could be true, such as being followed, poisoned, deceived by a spouse, or having a disease. This disorder does not generally involve any of the other symptoms of psychosis like hallucinations.
Substance Use Disorders
These disorders represent a significant public health issue, characterized by an individual’s compulsive use of substances despite harmful consequences. These disorders can disrupt an individual’s ability to function in daily life and are marked by a physical and psychological reliance on substances, including alcohol, tobacco, illicit drugs, and prescription medications. The complexity of these disorders involves a combination of behavioral, cognitive, and physiological phenomena.
- Alcohol – Disorders involving excessive alcohol consumption, leading to severe health issues, psychological problems, and social impairments.
- Cannabis – Includes problematic usage of marijuana and other cannabis-derived substances that may impair one’s ability to function properly in daily life.
- Opioids – Encompasses dependence on substances like heroin, as well as prescription pain relievers such as oxycodone, hydrocodone, and fentanyl. These are particularly notorious for their high potential for addiction and the risk of overdose.
- Stimulants – This category includes illicit drugs like cocaine and methamphetamine, as well as prescription stimulants such as amphetamines used to treat conditions like ADHD. Abuse can lead to severe psychological or physical dependence.
- Hallucinogens – Pertaining to the misuse of drugs that cause significant alterations in perception, mood, and cognitive processes, such as LSD, psilocybin, and peyote.
- Sedatives, Hypnotics, or Anxiolytics – Relates to misuse of prescription medications that cause calming or sleep-inducing effects, such as benzodiazepines and barbiturates, which can lead to severe dependence and withdrawal issues.
Trauma and Stressor-Related Disorders
These include a category of mental health conditions that arise as direct consequences of exposure to traumatic or intensely stressful situations. These disorders manifest through a variety of emotional and behavioral symptoms following events such as natural disasters, combat, personal assaults, or significant life transitions like divorce or the death of a loved one.
- Post-Traumatic Stress Disorder (PTSD) – This is a condition that affects countless people. The symptoms are quite difficult to manage and persist for years if left untreated. It can occur from any number of potential traumas such as physical abuse, sexual assault, car accidents, medical emergencies, natural disasters, or involvement in criminal events such as robberies or muggings to name just a few. PTSD can result when a person is exposed to death or threatened physical injury either through direct exposure, witnessing or through indirect exposure. If a number of these symptoms persist beyond one month following the traumatic event, it is likely to be PTSD.
- Acute Stress Disorder (ASD) – It shares many symptoms with PTSD, such as mood instability and severe anxiety, but its symptoms occur immediately after the trauma and last for a relatively short duration—from three days to up to one month. Early intervention is crucial for ASD and can prevent the development of PTSD.
- Adjustment Disorders are triggered by significant life changes or stressors that are overwhelming but not necessarily life-threatening. They are marked by symptoms like hopelessness, frequent crying, anxiety, changes in appetite, difficulty sleeping, and social withdrawal. Treatment typically involves psychotherapy and may include medications to alleviate the symptoms.
Overall, the diagnosis and treatment of trauma and stressor-related disorders require a comprehensive personal history and clinical assessment. Management is tailored to the individual, combining psychotherapy and pharmacotherapy to aid recovery and enhance the quality of life.
DIAGNOSIS & ASSESSMENT IN PSYCHIATRY
The treatment of mental health disorders relies on several foundational frameworks that guide clinicians in the accurate diagnosis and effective management of these conditions. Below is an explanation of key treatment frameworks that are integral to the field of psychiatry:
Diagnostic and Statistical Manual of Mental Disorders (DSM)
The Diagnostic and Statistical Manual of Mental Disorders, commonly known as the DSM, is a publication by the American Psychiatric Association that serves as a major authority for diagnosing mental disorders. The DSM contains descriptions, symptoms, and other criteria for diagnosing mental disorders. It ensures that a standard language and comprehensive guidelines are available to clinicians across the healthcare spectrum. The DSM’s systematic categorization helps in defining and communicating complex mental health conditions, which is crucial for treatment planning. It is regularly updated to reflect new scientific knowledge and changes in the understanding of mental health.
Psychiatric Evaluation and Assessment Tools
Psychiatric evaluation involves a detailed assessment of a person’s mental state to diagnose potential mental disorders and guide treatment decisions. This evaluation typically includes interviews, psychological testing, and physical examinations. Assessment tools may involve structured or semi-structured interviews, self-report questionnaires, behavioral observation, and sometimes neurophysiological testing. These tools gather comprehensive information about the individual’s symptoms, behavior, thought patterns, emotions, and overall functioning. These tools’ results help form a holistic view of the patient’s mental health, facilitating targeted treatment interventions.

Importance of Differential Diagnosis
Differential diagnosis is a critical process in the field of psychiatry that involves distinguishing a particular disease or condition from others that present similar clinical features. This process is fundamental because many mental health disorders share overlapping symptoms. For example, symptoms like anxiety and depression can occur in a variety of disorders and must be correctly identified to determine the most effective treatment plan. A differential diagnosis ensures that the treatment provided is appropriate to the specific conditions affecting the patient, which enhances treatment efficacy and patient safety.
Cultural Considerations in Diagnosis
Cultural considerations play a significant role in the diagnosis of mental health conditions. Cultural factors can influence the presentation of symptoms, the patient’s perception of their problems, their coping styles, and even their willingness to seek help. For instance, some cultures may express psychological distress through physical symptoms rather than emotional expressions. Additionally, cultural stigma can affect how symptoms are reported and perceived both by the patient and the clinician. Incorporating cultural considerations into the diagnostic process involves understanding and respecting the patient’s cultural background and adapting diagnostic methods and treatment interventions accordingly. This approach helps in providing culturally sensitive and effective care, which is more likely to be accepted and successful in diverse patient populations.
Together, these frameworks form a comprehensive approach to the assessment, diagnosis, and treatment of mental disorders. They emphasize the need for accuracy, thoroughness, and cultural sensitivity in the practice of mental health care.
MENTAL HEALTH PROVIDERS IN PSYCHIATRY
In the field of psychiatry and mental health, various types of professionals contribute to the assessment, diagnosis, treatment, and ongoing management of mental illnesses. Each type of mental health provider brings unique skills and expertise tailored to offer comprehensive care and support to individuals facing mental health challenges. Here is a detailed summary of the main types of mental health providers in psychiatry:
Psychiatrists
These are medical doctors who specialize in mental health and are qualified to diagnose and treat mental illnesses through a combination of medical, psychological, and social approaches. They have the authority to prescribe medications, which makes them unique among mental health professionals. Psychiatrists often manage treatment plans that may include medication, psychotherapy, and other interventions. They are also trained to understand the complex relationship between emotional and physical health and can treat severe mental health conditions such as schizophrenia, bipolar disorder, and major depression. The special education and training received includes:
- Medical Education: Psychiatrists, like family doctors, earned their medical degrees but had a focused concentration on a specialized field, in this case, the study and treatment of mental health conditions. Rather than just introductory courses on mental health disorders, psychiatrists take advanced and in-depth coursework specific to this area of study.
- Residency Training: After medical school, psychiatrists undertake an additional four-year program that involves intense clinical training under the direction and supervision of experienced psychiatrists in very specific settings. They learn the subtleties and intricacies of assessing, diagnosing, and treating mental health issues.
- Psychopharmacology: Unlike regular pharmacology coursework intended to educate doctors about all medications, psychiatrists have a specific concentration and focus on medicines designed to treat psychological issues. They possess much more refined skills in the action and mechanism of medications, side effects, and drug interactions than most doctors would have.
- Psychotherapy: Even psychiatrists have some limited experience and practice in performing psychotherapy. They can recognize environmental stressors that may be the underlying cause or driver of a person’s mental health problems and appropriately guide and help them with these issues.
- Assessment and Diagnosis: Psychiatrists perform a thorough clinical assessment that rivals that of a family doctor. This assessment is intended to pinpoint the issue in great detail and specificity.
- Crisis Intervention: Psychiatrists can assess the severity and risks that are sometimes associated with mental health issues. This could be determining if someone needs to be hospitalized due to suicidality, may have drug-induced disorders necessitating detox protocols, or medical conditions presenting as mental health that may need immediate attention.
Psychiatric Nurses
These individuals are registered nurses (RNs) or advanced practice registered nurses (APRNs) specializing in mental health nursing. They play a key role in the assessment and management of patients with mental health conditions, providing care in psychiatric wards, outpatient clinics, and community settings. Advanced practice psychiatric nurses, including clinical nurse specialists and nurse practitioners, can perform patient assessments and some may have prescribing authority depending on the state regulations.
Some people would prefer to see a psychiatric nurse practitioner instead of a psychiatrist for several reasons. In many states, there are more psychiatric nurse practitioners than there are psychiatrists, so often, people can get in sooner to see a psychiatric nurse practitioner. For people with a high deductible health plan, a psychiatric nurse practitioner is often a more cost-effective choice as their rates are a bit lower. Some people find psychiatric nurse practitioners have a friendlier interaction whereas some psychiatrists may be a bit more clinical and detached, however, bedside manner is often more specific to the person.
Each type of mental health provider offers distinct contributions to the treatment and support of individuals with mental health issues, and their roles often overlap and complement one another in multidisciplinary mental health care teams.
ACCESSING MENTAL HEALTH CARE
Accessing mental health care involves several key steps that can vary significantly depending on one’s geographical location, financial situation, and the severity of the condition. Here’s a detailed explanation of how to access mental health care across different avenues:
Finding a Provider
To find a mental health provider, such as a psychiatrist, psychologist, or therapist, you can start by consulting your primary care physician for a referral. Primary care doctors often have networks of specialists they can recommend. Another effective method is using online resources such as the websites of professional organizations (American Psychological Association, American Psychiatric Association, etc.), which typically offer directories of licensed practitioners. You can also consult your insurance provider for a list of covered providers. When selecting a provider, consider factors like their specialty, treatment philosophy, and patient reviews to ensure they align with your needs and preferences.
Psychiatrists and psychiatric nurse practitioners are specialists not typically in primary care clinics. Like cardiologists and dermatologists, most specialists locate themselves in private practices. Generally, larger mental health clinics have psychiatric providers on staff in conjunction with psychologists, professional counselors, and marriage and family therapists. This often provides one-stop shopping for many people. A client may see a psychiatrist for medication management and a therapist to work on building skills to stabilize further and eliminate their mental health issues. These providers will refer to each other to provide the best treatment possible for the client.
Insurance Coverage and Affordability
Understanding your insurance plan is crucial to accessing affordable mental health care. Contact your insurance provider to inquire about coverage specifics, including which mental health services are covered, whether you need referrals for specialist visits, what your copayments look like, and the specifics about in-network versus out-of-network benefits. If you lack insurance or find coverage insufficient, look for providers who offer sliding scale fees based on income, or seek services from nonprofits or academic institutions (many universities offer low-cost services provided by graduate students under supervision).
Telepsychiatry and Remote Services
Telepsychiatry provides an opportunity to access mental health services remotely via videoconferencing, phone calls, or text messaging, which is especially beneficial for those in remote areas or with limited mobility. Many mental health professionals have adapted to offer remote services, which can be accessed through private practices or specialized online platforms dedicated to mental health care. To use these services, check with existing or potential providers to see if they offer telepsychiatry options. These services often require a stable internet connection and a private space where you can talk without interruptions.
Who is Tele-Therapy for?
- Clients with schedules that are too busy to get away from the office.
- Clients with medical conditions preventing you from getting to our office.
- Couples or families who struggle to find times that work for everyone.
- Clients that simply prefer to do therapy from home.
- Clients who run into childcare, work conflicts, car problems, or weather concerns.
- Clients living in rural areas with limited services.
- Students going away to college somewhere in Minnesota.
- Clients with travel anxiety or agoraphobia.
Community Mental Health Centers
Community mental health centers are public or nonprofit entities that provide mental health services on a sliding scale fee basis. These centers often offer comprehensive care, including diagnosis, counseling, medication management, and support for individuals with serious mental illnesses. They are designed to be accessible and affordable, particularly for low-income individuals or those without insurance. You can find community mental health centers by searching online, checking with local health departments, or inquiring through social service agencies.
Community Mental Health Centers in Minnesota:
- HAMM Memorial Psychiatric Clinic:10 River Park Pl Ste 710, St. Paul
- Hennepin County Mental Health Center: 2215 East Lake Street, Minneapolis
- Face to Face Health & Counseling Service Inc.:1165 Arcade Street, Saint Paul, MN 55106, (651) 772-5555
- Family Services Rochester: 4600 18th Avenue NW, Rochester, MN 55901, (507) 287-2010
- Family Tree, Inc.:1619 Dayton Avenue, Suite 205, Saint Paul, MN 55104, (651) 645-0478
- Acacia Counseling & Wellness:2724 University Ave SE, Minneapolis, MN 55414, (612) 299-1090
- Alliance Wellness Center:8040 Old Cedar Ave S #101, Bloomington, MN 55425, (952) 562-3740
- Avivo:1900 Chicago Ave., Minneapolis, MN 55404, (612) 752-8000
- Minnesota Mental Health Clinics:7 clinic locations serving Minneapolis & Saint Paul Metro Area, (651) 454-0114
Crisis Intervention and Hotlines
In times of a mental health crisis, immediate assistance can be accessed through various hotlines and crisis intervention services. In the United States, the Suicide and Crisis Lifeline can be reached by dialing 988, providing 24/7 support to those in distress. Additionally, many communities have mobile crisis teams that can provide in-person crisis services. These services are crucial for de-escalating situations and can guide you toward longer-term support solutions. Always keep local crisis numbers handy for immediate access in emergencies.
Crisis hotlines in Minneapolis, Minnesota:
- 988 Suicide and Crisis Lifeline: 988 for free and confidential emotional support 24/7
- Crisis Text Line: Text HOME to 741741 for free help 24/7, or AYUDA for Spanish
- MN Crisis Text Line: Text “MN” to 741741
- Mpls Suicide Crisis Hotline: 612-379-1199
- Men’s Crisis Line: 612-379-6367
- Hennepin County Child Crisis Team: 612-348-2233 for anyone 17 and under in crisis 24/7
- Minneapolis Public Schools mental health support hotline: 612-767-4158 Monday through Friday from 9 AM to 5 PM
- Community Outreach for Psychiatric Emergencies (COPE): 612-596-1223 for emergency intervention services 24/7
RESOURCES
For those seeking a psychiatrist, a variety of resources are available to guide them through the process of finding and choosing the right mental health professional. Here’s a summary of different types of resources, including books, guides, and online tools:
Books
- The Insider’s Guide to Mental Health Resources Online – by John M. Grohol: This book provides a comprehensive list of online resources for mental health, including directories and reviews of mental health professionals.
- Prescription for Psychiatry: Why We Need a Whole New Approach to Mental Health and Wellbeing – by Peter Kinderman: While not a direct guide to finding a psychiatrist, this book discusses the landscape of psychiatric care and could help individuals understand what to look for in psychiatric treatment.
Guides
- How to Find a Good Psychiatrist – Many mental health organizations publish guides on finding a psychiatrist, outlining steps to identify one’s needs, verifying credentials, and understanding treatment philosophies.
- NAMI (National Alliance on Mental Illness) – NAMI offers comprehensive guides that help individuals understand when to seek help, what kinds of psychiatrists are available, and how to manage their health care.
- APA (American Psychiatric Association) – The APA provides guidelines and a psychiatrist finder tool to help patients find a psychiatrist who suits their personal and medical needs.
Online Resources
- Psychiatrist Finders – Tools like the APA’s psychiatrist finder or Psychology Today’s therapist directory allow users to search for psychiatrists by location, specialty, and insurance acceptance.
- Patient Reviews – Websites like Healthgrades and ZocDoc enable patients to read reviews of psychiatrists and book appointments online.
- Mental Health Forums and Communities -Platforms like Reddit, Mental Health America, and The Mighty offer community support where individuals can share experiences and recommendations.

Specialty Organizations
- Child and Adolescent Psychiatry – The American Academy of Child and Adolescent Psychiatry offers a tool to find child and adolescent psychiatrists and provides resources specific to younger populations.
- Geriatric Psychiatry – The American Association for Geriatric Psychiatry provides resources and a directory for finding specialists who work with older adults.
These resources provide a solid starting point for anyone looking to find a psychiatrist that fits their needs and expectations. They help demystify the process and equip individuals with the necessary tools to make informed decisions about their mental health care.
