Table of Contents
INTRODUCTION
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after a person experiences or witnesses a traumatic event. Such events can include natural disasters, serious accidents, terrorist acts, war/combat, rape, or other violent personal assaults. PTSD is characterized by intense, disturbing thoughts and feelings related to the traumatic experience that persist long after the event has ended. These can manifest through flashbacks, nightmares, severe anxiety, and uncontrollable thoughts about the event.
Understanding PTSD is crucial for several reasons:
- Recognition and Support – Knowing the signs and symptoms of PTSD helps in recognizing it in oneself or others, facilitating early intervention and support.
- Reducing Stigma – Education about PTSD helps reduce the stigma associated with mental health conditions, encouraging more people to seek help without feeling ashamed.
- Effective Treatment – Awareness of PTSD leads to better treatment approaches, as individuals and healthcare providers can tailor interventions to meet specific needs.
- Improving Quality of Life – Understanding PTSD and its impact can improve the quality of life for those affected by promoting healthier coping mechanisms and support systems.
- Public Health Awareness – Raising awareness about PTSD can lead to broader public health initiatives and policies aimed at supporting mental health and addressing the needs of those affected by trauma.
Current Statistics on PTSD
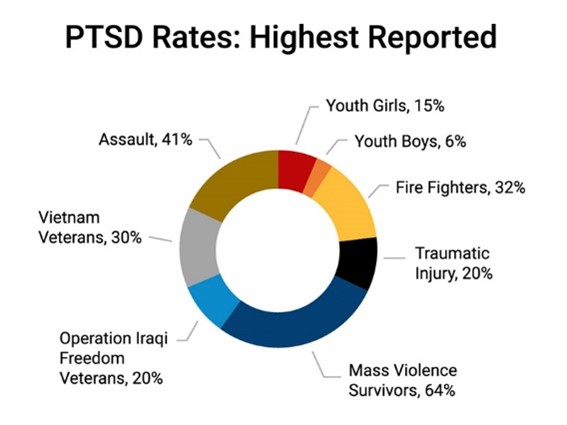
PTSD affects millions of people worldwide. Approximately 3.5% of adults in the United States experience symptoms each year. Lifetime prevalence is about 7-8% of the population. Women are more likely to develop PTSD than men, with about 10% of women and 4% of men experiencing it at some point in their lives. Additionally, an estimated 20% of veterans who served in Iraq and Afghanistan have PTSD.
Populations Most Affected
Certain populations are more vulnerable to PTSD due to their increased exposure to traumatic events. These groups include military veterans, first responders, survivors of physical and sexual assault, individuals involved in accidents or natural disasters, and refugees. Women are also at a higher risk, partly due to higher rates of sexual violence. Children and adolescents who experience or witness traumatic events are also significantly affected, often carrying symptoms into adulthood.
Source: University of Maryland
Causes of PTSD
PTSD can result when a person is exposed to death or threatened physical injury either through direct exposure, witnessing or through indirect exposure. If a number of these symptoms persist beyond one month following the traumatic event, it is likely to be PTSD.
Most people will experience at least one intrusive symptom:
- Unwanted upsetting memories
- Nightmares
- Flashbacks
- Emotional distress after exposure to traumatic reminders
- Physical reactivity after exposure to traumatic reminders
Most people also experience avoidant symptoms. This involves avoidance of trauma-related stimuli after the trauma:
- Trauma-related thoughts or feelings
- Trauma-related external reminders
Additionally, most people with PTSD will experience negative alterations in thinking and mood such as:
- Inability to recall key features of the trauma
- Overly negative thoughts and assumptions about oneself or the world
- Exaggerated blame of self or others for causing the trauma
- Negative affect
- Decreased interest in activities
- Feeling isolated
- Difficulty experiencing positive affect
Lastly, people with PTSD usually have some alterations in arousal and reactivity that can include:
- Irritability or aggression
- Risky or destructive behavior
- Hypervigilance
- Heightened startle reaction
- Difficulty concentrating
- Difficulty sleeping
UNDERSTANDING PTSD
Post-Traumatic Stress Disorder (PTSD) can develop after exposure to any number of traumatic events that can happen to people. Some common types of traumatic events that can result in PTSD include military combat, physical or sexual assaults, accidents, or natural disasters such as a tornado, hurricanes, etc. Although PTSD has likely existed since humankind has been involved in traumatic situations, PTSD has only been recognized as a diagnosis since 1980. It should be noted that not everyone who experiences a traumatic event will end up with PTSD. Many people endure and recover from difficult life situations just fine. Others develop less severe problems such as depression or anxiety problems. Traumatic events that are enduring (military combat) or recurring (physical or sexual abuse) increase the likelihood of developing PTSD.
Criteria for Diagnosis
The diagnosis of PTSD is based on specific criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The criteria include:
- Exposure to Trauma – Directly experiencing, witnessing, learning about, or being repeatedly exposed to details of a traumatic event.
- Intrusive Symptoms – Presence of one or more symptoms such as distressing memories, nightmares, flashbacks, or intense psychological distress at exposure to cues related to the trauma.
- Avoidance – Persistent avoidance of reminders associated with the traumatic event, including thoughts, feelings, people, places, and activities.
- Negative Changes in Cognition and Mood – Two or more symptoms such as memory problems related to the trauma, negative beliefs about oneself or the world, distorted blame, persistent negative emotional state, diminished interest in activities, feelings of detachment, or inability to experience positive emotions.
- Arousal and Reactivity – Two or more symptoms such as irritability, reckless or self-destructive behavior, hypervigilance, exaggerated startle response, concentration difficulties, or sleep disturbances.
- Duration – Symptoms must persist for more than one month.
- Functional Impairment – The symptoms cause significant distress or impairment in social, occupational, or other important areas of functioning.
- Exclusion – The disturbance is not attributable to the physiological effects of a substance or another medical condition.
A diagnosis is typically made by a qualified mental health professional through a comprehensive clinical evaluation, which may include a detailed patient history and the use of standardized assessment tools.
Types of PTSD
- Acute PTSD – It is a type of post-traumatic stress disorder that occurs within the first three months following exposure to a traumatic event. Individuals with acute PTSD experience intense and disruptive symptoms such as flashbacks, nightmares, avoidance behaviors, and heightened arousal. These symptoms must persist for at least one month but less than three months. Early intervention and treatment can be highly effective in managing acute PTSD and preventing it from becoming chronic.
- Chronic PTSD – It is diagnosed when symptoms of post-traumatic stress disorder persist for more than three months following the traumatic event. Symptoms may include recurring intrusive memories, avoidance of reminders of the trauma, negative changes in thought patterns and mood, and increased arousal and reactivity. Chronic PTSD can significantly impair an individual’s ability to function in daily life and may require long-term treatment and support to manage the symptoms effectively.
- Complex PTSD (C-PTSD) – It results from prolonged or repeated exposure to traumatic events, such as long-term abuse, captivity, or torture. It encompasses the core symptoms of PTSD but also includes additional symptoms such as difficulties with emotional regulation, persistent feelings of hopelessness, distorted perceptions of the perpetrator, and problems with interpersonal relationships. Complex PTSD often requires specialized and extended therapeutic interventions to address the multifaceted impact of long-term trauma on an individual’s mental health and well-being.

Source: Oro House
Causes and Risk Factors of PTSD
Post-Traumatic Stress Disorder (PTSD) is a mental health condition triggered by experiencing or witnessing a traumatic event. It can lead to severe anxiety, flashbacks, nightmares, and uncontrollable thoughts about the event. Below is a summary of the causes and risk factors associated with PTSD:
Traumatic Events Leading to PTSD
- Combat Exposure – Military personnel and veterans face high risks due to exposure to combat and life-threatening situations.
- Natural Disasters – Events such as earthquakes, hurricanes, and floods can lead to PTSD.
- Serious Accidents – Major car crashes or other life-threatening accidents.
- Violent Assaults – Experiences of physical or sexual assault, robbery, or other violent attacks.
- Childhood Abuse – Physical, emotional, or sexual abuse during childhood.
- Serious Health Problems – Life-threatening illnesses or medical procedures, particularly those experienced in childhood.
- Sudden Death of a Loved One – Unexpected loss of a close family member or friend.
Genetic and Environmental Factors
- Genetic Predisposition – A family history of mental health issues can increase susceptibility to PTSD.
- Brain Structure and Function – Variations in brain areas that regulate emotions and fear responses.
- Environmental Factors – Prolonged exposure to stress, lack of support systems, and previous traumatic experiences.
The top risk factors encompass a combination of the severity and duration of traumatic events, personal and family mental health history, demographic factors, occupational hazards, social support systems, and substance abuse. Individuals exposed to severe or prolonged trauma, such as combat veterans or those who experienced childhood abuse, are particularly vulnerable. A personal or family history of mental health issues can further increase the risk. Women are generally at a higher risk, possibly due to greater exposure to sexual violence. Occupations like first responders and healthcare workers, who frequently encounter traumatic situations, also face elevated risks. Moreover, a lack of social support and social withdrawal after trauma can exacerbate the condition. Lastly, substance abuse, including alcohol and drugs, significantly heightens the susceptibility to developing PTSD and can worsen its symptoms.
SYMPTOMS & DIAGNOSIS
In response to a traumatic experience where real or perceived life-threatening situations have occurred, people experience some of the following symptoms. There are re-experiencing symptoms that include: 1) intrusive thoughts or images, 2) feeling like the event is recurring or reliving it, 3) dreams or nightmares, 4) psychological distress at exposure to cues that resemble the event, 5) physical reaction on exposure to things that resemble the event. There are avoidant symptoms that include: 1) avoiding thinking about the event, 2) avoiding activities that remind you of the event, 3) inability to recall parts of the event, 4) being detached or estranged from others, 5) loss of interest in normal activities, 6) feeling numb, 7) little hope for the future. Finally, some symptoms of heightened arousal include: 1) disturbed sleep, 2) irritability, 3) indecisiveness or lack of concentration 4) hypervigilance, 5) exaggerated startle response.
Intrusive Memories
One of the hallmark symptoms of PTSD is the presence of intrusive memories. These are recurrent, unwanted distressing memories of the traumatic event that can invade a person’s mind at any time. Individuals may experience flashbacks, in which they feel as though they are reliving the traumatic event. This can be incredibly distressing and disorienting, often accompanied by intense emotional and physical reactions. Nightmares related to traumatic events are also common, causing disturbed sleep and heightened anxiety.
Avoidance Behaviors
To cope with distressing memories and emotions, individuals with PTSD often engage in avoidance behaviors. This can involve avoiding thoughts or conversations about the traumatic event, as well as steering clear of places, activities, or people that might trigger memories of the trauma. For instance, someone who has experienced a car accident might avoid driving or even riding in a car. This avoidance can significantly impact daily functioning and lead to isolation.
Negative Changes in Thinking and Mood
PTSD can also bring about negative changes in thinking and mood. Sufferers might develop persistent negative thoughts about themselves, others, or the world around them. They may feel hopeless about the future and experience a sense of emotional numbness. This can result in a loss of interest in activities they once enjoyed and feelings of detachment from friends and family. Such negative shifts in cognition and mood can exacerbate feelings of depression and anxiety.
Changes in Physical and Emotional Reactions
Lastly, PTSD often causes changes in physical and emotional reactions, also known as arousal symptoms. These can include being easily startled or frightened, always being on guard for danger (hypervigilance), and experiencing trouble sleeping or concentrating. Individuals might also display irritability, angry outbursts, or aggressive behavior. These heightened reactions are the body’s way of remaining prepared to respond to perceived threats but can lead to chronic stress and physical health issues over time.
Understanding these symptoms is crucial for recognizing PTSD in oneself or others. If you or someone you know is struggling with PTSD, it’s important to seek professional help. Therapy, medication, and support from loved ones can play a vital role in managing and overcoming the symptoms of PTSD.
Diagnosis of PTSD
Post-Traumatic Stress Disorder (PTSD) is diagnosed based on the criteria outlined in the DSM-5, which include experiencing or witnessing a traumatic event, recurrent distressing memories, flashbacks, nightmares, avoidance behaviors, negative changes in cognition and mood, and alterations in arousal and reactivity. These symptoms must persist for more than one month and cause significant distress or impairment in functioning.
Assessment tools and screenings are essential in diagnosing PTSD. The Clinician-Administered PTSD Scale (CAPS) is a structured interview used to diagnose PTSD and assess its severity. The PTSD Checklist for DSM-5 (PCL-5) is a self-report measure that evaluates the presence and severity of PTSD symptoms. Other tools, like the Impact of Event Scale-Revised (IES-R) and the PTSD Symptom Scale Interview (PSS-I), are also used to assess the impact and severity of PTSD symptoms.
Healthcare professionals play a crucial role in diagnosing and managing PTSD. They conduct comprehensive assessments using standardized tools, evaluate the patient’s history and symptoms, and develop individualized treatment plans. These plans may include evidence-based therapies such as Cognitive Behavioral Therapy (CBT), Eye Movement Desensitization and Reprocessing (EMDR), and medication management. Healthcare professionals also provide education and support to patients and their families, monitor progress, and make necessary adjustments to treatment plans to ensure effective management and recovery from PTSD.
TREATMENT OPTIONS
Post-Traumatic Stress Disorder (PTSD) is treated through various therapies and medications. Cognitive Behavioral Therapy (CBT) focuses on changing negative thought patterns and behaviors related to trauma. This therapy helps patients understand and reframe their thoughts, reducing the impact of trauma on their daily lives. Eye Movement Desensitization and Reprocessing (EMDR) combines elements of cognitive therapy with bilateral sensory input, such as guided eye movements, to help patients process and reframe distressing memories. Prolonged Exposure Therapy involves patients confronting their traumatic experiences in a controlled setting, which helps reduce the fear and anxiety associated with these memories.
EMDR
Many people have endured difficult, painful, and traumatic events or experiences in their lives. For many, the mental and emotional fallout is long-lasting and dramatically interferes with normal functioning. EMDR (Eye Movement Desensitization and Reprocessing) is a specialized type of psychotherapy that helps people heal from these experiences in a fraction of the time of traditional therapy. Research studies find that 72% of combat vets and people with multiple or repeated trauma no longer met the criteria for PTSD after just 6-12 sessions of EMDR. Over the past 25 years millions of people have received successful treatment with EMDR.
EMDR is generally an eight-phase treatment process. During the intake, your clinician gets a thorough history and begins to identify traumatic memories to target. Before tackling any trauma, your therapist will help work on teaching new strategies and methods for coping with emotional and mental stress. When ready to tackle some of the traumatic memories, some parts of the session will include eye movements (or some bilateral stimulation). Experts believe this activity is connected to biological mechanisms in REM sleep that facilitate the processing of disturbing memories and feelings. Many people feel EMDR helps them get “unstuck” so they can heal and move past their troubling memories and events. Many also report feeling empowered over the experiences that once debased and haunted them. These wounds finally begin to transform so people can resume living their lives.
Therapeutic Medications
Medications prescribed for PTSD typically include:
- Antidepressants – Selective serotonin reuptake inhibitors (SSRIs) such as sertraline (Zoloft) and paroxetine (Paxil) are commonly prescribed. These medications help alleviate symptoms of depression and anxiety associated with PTSD. Other types of antidepressants, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) like venlafaxine (Effexor), may also be used.
- Anti-anxiety Medications – Benzodiazepines, such as clonazepam (Klonopin) and lorazepam (Ativan), may be prescribed for short-term relief of severe anxiety symptoms. However, these medications are generally used with caution due to their potential for dependence and abuse.
- Prazosin – This medication is specifically used to treat nightmares and sleep disturbances related to PTSD. Prazosin helps reduce the frequency and intensity of nightmares, leading to better sleep quality.
- Atypical Antipsychotics – Medications such as risperidone (Risperdal) and quetiapine (Seroquel) might be prescribed, especially for patients who do not respond adequately to antidepressants alone or have additional symptoms such as severe agitation or mood swings.
- Mood Stabilizers – Medications such as lamotrigine (Lamictal) and valproic acid (Depakote) may be used to help stabilize mood and reduce symptoms such as irritability and anger outbursts.
These medications are often used in combination with psychotherapy to provide comprehensive treatment for PTSD. In fact, psychotherapy focuses on educating sufferers about the condition and helps them understand that it results not from weakness but extraordinary stress. Cognitive-behavioral therapy helps address inaccurate ways of thinking about the trauma. Eye movement desensitization reprocessing (EMDR) is a new type of psychotherapy that has gained some support as a method of helping people work through trauma. Psychotherapy helps sufferers of PTSD address five core needs crucial to all people: safety, trust, control, esteem, and intimacy.
Alternative Treatments
Alternative treatments for PTSD provide additional options beyond traditional therapy and medications, aiming to address the condition holistically. These treatments often focus on the mind-body connection and can be used alongside conventional approaches for a more comprehensive care plan.
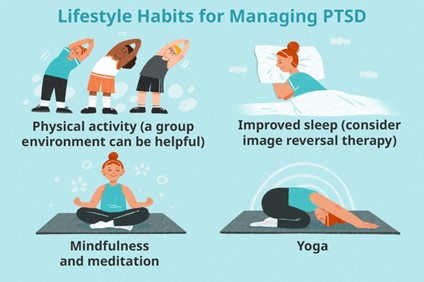
Mindfulness and meditation practices help individuals develop awareness and acceptance of their thoughts and feelings, reducing stress and improving emotional regulation. Yoga, with its emphasis on breath control, meditation, and physical postures, can help alleviate symptoms by promoting relaxation and enhancing body awareness.
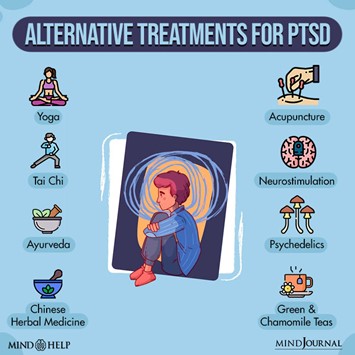
Acupuncture, an ancient Chinese medicine practice, involves inserting thin needles into specific points on the body to balance energy flow and reduce symptoms of anxiety and depression. Art therapy allows individuals to express and process their emotions through creative activities, providing a non-verbal outlet for trauma-related feelings.
Animal-assisted therapy, involving interactions with animals such as dogs or horses, can reduce stress and promote feelings of safety and comfort. Service dogs specifically trained to assist with PTSD can provide emotional support and help manage symptoms in everyday situations
Nutritional and dietary interventions focus on the impact of diet on mental health, with some evidence suggesting that a balanced diet rich in omega-3 fatty acids, vitamins, and minerals can support overall brain health and improve PTSD symptoms.
Lastly, physical exercise is a powerful tool in managing PTSD, as it helps reduce stress, improve mood, and increase overall well-being. Regular physical activity has been shown to decrease anxiety and depression symptoms, making it a valuable component of a holistic treatment plan.
These alternative treatments offer diverse and complementary approaches to managing PTSD, supporting individuals in finding the most effective and personalized path to recovery.
LIVING WITH PTSD
Common PTSD coping strategies include various techniques and lifestyle choices designed to manage stress, promote well-being, and build a support network. Stress management techniques such as mindfulness and meditation help individuals stay grounded and reduce intrusive thoughts, while deep breathing exercises, like 4-7-8 breathing, can promote relaxation and alleviate anxiety. Grounding techniques, which involve focusing on physical sensations and immediate surroundings, keep individuals connected to the present moment. Regular physical activity, such as walking, running, yoga, or tai chi, is beneficial for improving mood and reducing stress. Professional therapy, including Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR), offers structured approaches to managing PTSD symptoms.
Healthy lifestyle choices are also crucial for coping with PTSD. Maintaining a balanced diet rich in fruits, vegetables, lean proteins, and whole grains supports overall health, while adequate sleep, achieved through a regular sleep schedule and a calming bedtime routine, enhances sleep quality. Staying hydrated and limiting alcohol and recreational drug use can prevent the exacerbation of PTSD symptoms, and regular medical check-ups help address physical health concerns that might contribute to stress.
Building a support network is another key aspect of coping with PTSD. Open communication with trusted family members and friends provides emotional support, while joining support groups, either in-person or online, offers a sense of community and shared understanding. Professional support from mental health professionals provides tailored coping strategies and ongoing assistance. Utilizing community resources, such as local mental health organizations and crisis centers, offers additional support services. Finally, self-help resources like books, podcasts, and online materials focused on PTSD and trauma recovery provide valuable insights and coping strategies.
Impact on Daily Life
The impact of PTSD on daily life can be profound and multifaceted, affecting work, relationships, the management of triggers and flashbacks, and the necessity of seeking accommodations.
In the workplace, individuals with PTSD often struggle with concentration, memory issues, and maintaining productivity. The heightened anxiety and hypervigilance associated with PTSD can make it difficult to stay focused on tasks, leading to reduced efficiency and increased errors. These challenges can result in frustration and a sense of inadequacy, potentially causing individuals to withdraw from workplace interactions or avoid seeking career advancement opportunities. Relationships with colleagues can also be strained due to irritability, emotional numbness, or avoidance behaviors, which others may misunderstand as disinterest or hostility.
Personal relationships are similarly impacted. The symptoms of PTSD, such as emotional detachment, hyperarousal, and irritability, can create barriers to intimacy and communication. Loved ones may feel confused or hurt by the individual’s emotional withdrawal or sudden outbursts. This can lead to misunderstandings, conflicts, and a sense of isolation for both the individual with PTSD and their family or friends. Maintaining healthy relationships requires significant effort and understanding from all parties involved, often necessitating therapy or counseling to navigate these challenges effectively.

Managing triggers and flashbacks is a continuous and demanding aspect of living with PTSD. Triggers can be specific sounds, smells, places, or even people that remind the individual of the traumatic event. When triggered, the person may experience intense flashbacks, where they feel as if they are reliving the trauma. This can be incredibly distressing and disruptive to daily activities. Learning to identify and manage these triggers through grounding techniques, deep breathing exercises, and mindfulness practices is crucial. Grounding techniques might include focusing on physical sensations, such as the texture of an object or the feeling of feet on the ground, to bring the individual back to the present moment.
Seeking accommodations at work or school is often necessary to create a supportive environment that allows individuals with PTSD to function effectively. Accommodation might include flexible scheduling to accommodate therapy appointments or times when symptoms are particularly severe. Providing a quiet and less stimulating work environment can help reduce stress and anxiety. Allowing for additional breaks can give the individual time to practice coping strategies when feeling overwhelmed. Communicating openly with employers or educational institutions about PTSD and the specific needs for accommodations can help foster a supportive atmosphere, reducing the stigma and making it easier for individuals to seek the help they need.
Overall, the impact of PTSD on daily life is significant, requiring ongoing management and support. By understanding these challenges and implementing strategies to address them, individuals with PTSD can improve their quality of life and maintain better functionality in their personal and professional lives.
RESEARCH & FUTURE DIRECTION
Ongoing Studies and Clinical Trials
Researchers are actively engaged in numerous studies and clinical trials to better understand PTSD and develop more effective treatments. These studies often focus on identifying the underlying mechanisms of PTSD, evaluating the efficacy of various therapeutic approaches, and exploring new treatment modalities. Clinical trials are crucial for testing the safety and effectiveness of emerging therapies, including pharmacological interventions, psychotherapeutic techniques, and innovative combinations of both.
Advances in Treatment Approaches
Recent advances in PTSD treatment include a range of pharmacological and non-pharmacological strategies. New medications are being developed and tested to target specific symptoms of PTSD, such as hyperarousal and intrusive memories. In the realm of psychotherapy, techniques like Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) continue to be refined. Additionally, integrative approaches that combine medication with therapy, as well as novel therapies like ketamine-assisted psychotherapy and MDMA-assisted therapy, are showing promise in clinical trials.
Role of Technology in PTSD Treatment
Technology is playing an increasingly important role in PTSD treatment. Virtual reality (VR) is being used to create controlled environments for exposure therapy, allowing individuals to confront and process traumatic memories in a safe and structured manner. Mobile health applications and teletherapy platforms are making mental health services more accessible, especially for those in remote or underserved areas. These technologies offer convenience and anonymity, which can reduce the stigma associated with seeking help.
Emerging Therapies
Future therapies for PTSD are likely to include a broader range of pharmacological and psychotherapeutic options. Advances in neuroscience and pharmacology may lead to the development of drugs that more precisely target the neurobiological underpinnings of PTSD. Additionally, therapies involving psychedelics, such as psilocybin and MDMA, are gaining attention for their potential to facilitate profound therapeutic experiences and long-term symptom relief.
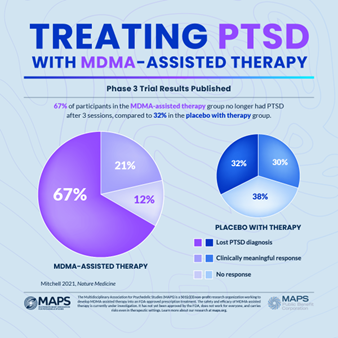
Source: MAPS.org
Innovations in Diagnostic Tools
Innovations in diagnostic tools are expected to enhance the accuracy and timeliness of PTSD diagnosis. Biomarkers, such as genetic, epigenetic, and neuroimaging markers, may provide objective measures for diagnosing PTSD and predicting treatment responses. These advancements could lead to more personalized treatment plans and better outcomes for individuals with PTSD.
Public Awareness and Education Efforts
Increasing public awareness and education about PTSD is essential for reducing stigma and encouraging individuals to seek help. Efforts include public campaigns, educational programs in schools and workplaces, and training for healthcare providers to better recognize and address PTSD. By raising awareness, society can create a more supportive environment for those affected by PTSD.
Resources Available for Those Affected by PTSD
A growing array of resources is becoming available to support individuals with PTSD and their families. These resources include support groups, both in-person and online, educational materials, and access to mental health professionals. Organizations dedicated to PTSD research and advocacy are also expanding their outreach and services, providing critical support and information to those in need.
In conclusion, the field of PTSD research and treatment is rapidly evolving, with ongoing studies and clinical trials contributing to significant advancements in our understanding and management of the disorder. Future directions hold promise for emerging therapies, innovative diagnostic tools, enhanced public awareness, and a wealth of resources to support those affected by PTSD. Through continued research and collaboration, we can hope to achieve better outcomes and improve the quality of life for individuals living with PTSD.
SUPPORT & RESOURCES
National Institute of Mental Health (NIMH)
Provides comprehensive information on PTSD, research updates, and resources for finding help.
Offers educational resources, self-help tools, and information on treatment options.
American Psychological Association (APA)
Provides information on PTSD treatment guidelines and finding a psychologist.
Anxiety and Depression Association of America (ADAA)
Offers resources on PTSD, including treatment options and a directory of mental health professionals.

An online community where individuals with PTSD can share experiences and support each other.
Daily Strength PTSD Support Group
An online support group where members can discuss their challenges and find support.
Hotlines and Emergency Contacts
National Suicide Prevention Lifeline
24/7 support for people in distress, prevention, and crisis resources. Phone: 1-800-273-8255
Confidential help for Veterans and their families. Available 24/7. Phone: 1-800-273-8255 and press 1, or text 838255
Free, confidential, 24/7 treatment referral and information service. Phone: 1-800-662-HELP (4357)
Provides free, 24/7 support via text message. Text “HELLO” to 741741

These resources provide various forms of support, from professional treatment to peer connections and immediate crisis intervention. If you or someone you know is struggling with PTSD, reaching out to one of these resources can be an important step towards healing and recovery.